
Veteran Mental Health: Surprising Facts and Figures that Should be Addressed

Mental health is as important as keeping one’s physical, emotional, and spiritual wellness. With this, we have thought of identifying the common concerns and issues regarding our veteran’s mental health.
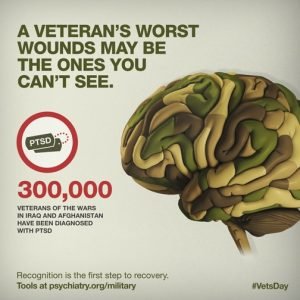
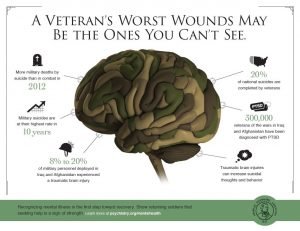
RAND Center for Military Health Policy Research reported that 20% of all vets who served in Afghanistan or Iraq suffered from post-traumatic stress disorder or major depression. Also, 19.5% of that same group of vets also suffered a traumatic brain injury. These three disorders related to military service alone have a major impact need for mental health treatment of veterans.
These mental health services for veterans are essential for helping our returning military vets recover from mental health issues and combat experiences related to their time in military service.
Mental Health Treatment Barriers Veterans May Face
The U.S. Department of Veterans Affairs has provided mental health treatment to 2.1 million veterans during the period between 2006 and 2010, according to the U.S. Government Accountability Office. The Substance Abuse and Mental Health Services Administration also conducted a study which showed that 50% of these returning vets in need of veteran mental health treatment do indeed receive the service.
This 50% statistic happens due to barriers both veterans and active service members face in search for mental health treatment. According to USGAO, these barriers include but are not limited to:
 Personal embarrassment for mental disabilities in need of professional help
Personal embarrassment for mental disabilities in need of professional help- Waiting for long periods of time to receive the treatment for these mental health issues
- The feeling of shame for requiring mental health treatment
- Being afraid of showing weakness
- Stigma associated with mental health issues
- Insufficient understanding or awareness for mental health issues and treatment methods
- Problems with logistics, like traveling long distances to receive these types of treatments
- Concerns about the treatment itself offered by the VA for veteran mental health
- False perceptions caused by demographic barriers on such things as gender or age
The American Psychological Association reported that in 2005 alone 22% of the veterans did apply for veteran mental health treatment provided by the private practices instead of seeking treatment from the VA. This number increased parallel to the increase in wait times in VA mental health facilities all around the country.
Veteran Mental Health and Substance Abuse
Substance abuse is an important part of veteran mental health and its treatment. The National Institute of Drug Abuse reported that the veterans’ combat exposure is strongly affecting their substance abuse inclinations. One particular study even showed that one quarter of the total Afghanistan and Iraq returning veterans, 25%, show signs of substance abuse disorder.
A majority of the calls we at the National Veterans Foundations handle do begin with loneliness and isolation issues. Without treatment, this may lead to problems with substance abuse, violent behavior, and relationship problems.
The NIDA also conducted a study in 2008 which showed that Army veterans and active duty personnel abused prescription drugs at two-times the rate prescribed for the civilian population.
An estimate issued by the VA in 2009 showed that approximately 13,000 veterans from Afghanistan and Iraq show alcohol dependence syndrome and are in need of veteran mental health treatment.
The Link between TBI and PTSD
The New England Journal of Medicine performed a survey that identified a link between traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD). The evidence showed that military members who experienced a traumatic brain injury were more than twice as likely to suffer from PTSD later on than service members who did not suffer a TBI. The PTSD onset was generally 3-4 months after returning from deployment.
Identifying the need for veteran mental health treatment is also an important part of the healing process. Veterans who are newly released may also have a period of delay between they experience any severe TBI and PTSD symptoms. Older vets, however, may show symptoms of the PTSD many years after discharge which are in need of extensive treatment.
Veterans Health Care Funding Needs to be Augmented

Mental health symbol conceptual design isolated on white background
The mental health care for veterans is in need of increased funding in order for every veteran to get the care they need, at the time of need it. Also, our veterans must never become political pawns used for budget battles, and the increasing wait times VA facilities face is what needs to be addressed and reduced through proper funding.
Insufficient funding of the mental health care system for our veterans can’t be ignored any longer. The men and women of this group have shown sacrifice and risked their lives for the protection of our people and country, so the least we should do is to ensure they get the mental health treatment services they need after discharge from the Army.
Here are some surprising facts about our troops’ mental health:
DoSomething.org reported that 5.5 million people, mostly youngsters, are making a positive change, on and offline. These facts and figures presented in the following text should help us realize the importance of taking actions ASAP.
PTSD, or post-traumatic stress disorder (an anxiety disorder which follows after experiencing a traumatic occurrence), and depression are the two #1 most common mental health issues affecting returning troops.
Most common PTSD symptoms include lack of interest, difficulty in concentrating, apathy, detachment feelings, lack of appetite, exaggerated startle response, sleep disorders (oversleeping or lack of sleep), and hypervigilance.
It takes several weeks of experiencing continued symptoms for a confirmed diagnosis of post-traumatic stress disorder.
11 to 20% of all Afghanistan and Iraq veterans, who participated in Operation Enduring Freedom and Operation Iraqi Freedom, are diagnosed with PTSD. A good way to contribute is to create a PTSD and/or other illnesses support board, open for all your friends who can participate by leaving messages intended for troops, to show their encouragement and support.
Three to four months after returning home, 30% of soldiers show mental problem development.
Launch a campaign and help make the world suck less!
38% of men and 55% of women also reported being victims of harassment and abuse during their time of military service.
Over 50% of the total number of people experiencing abuse in the military are men, due to the fact that there are more male soldiers than female.
20% of all Afghanistan and Iraq returning veterans succumb to drugs or heavy drinking after they come home to the U.S.
The number of Afghanistan and Iraq veterans suffering from a TBI (traumatic brain injury) is between 10 and 20%. This internal injury may possibly cause suicidal thoughts, anger, and personality changes as consequences.
22 veterans on average committed suicide every day in 2010. The largest group was comprised of men between 50 and 59 years of age.
Hispanics and African-American groups are possibly more likely to develop PTSD than whites.
More inLifestyle
-
`
A Veteran’s Open Letter To The Prince Of Cambridge
If you were born a prince, like a famous Prince of Cambridge, you would have a lot of options for your...
June 5, 2023 -
`
You Must Appreciate the Amazing Growth of the Tulsa Community Foundation
The Tulsa Community Foundation (TCF) is a charitable organization which was founded on the 30th of December 1998 by a banker,...
June 5, 2023 -
`
ELDERBERRIES: Learn about These Powerful, Immune-Strengthening Tart Little Fruits!
What would you do if someone handed you a capsule that could regulate your blood sugar level, help you lose weight,...
June 5, 2023 -
`
Here Is Why Lucy Kennedy Should Be Your Inspiration
For normal people like us, celebrities (or famous people, for that matter) offer a window to the limitless possibilities which we...
June 5, 2023 -
`
If You’re Among The Health-Watchers, You Should Probably Know About Pre-Diabetes
If you’re an adult and consider yourself sufficiently aware, you know what diabetes is. The disease is so common that even...
June 2, 2023 -
`
Motivation Isn’t Enough to Get You to the Finish Line; You Need Discipline!
Motivation is the intrinsic spirit to undertake a challenging task. It is the positive enforcement that comes from within and keeps...
June 2, 2023 -
`
Gardening and Green Activities: a Definite Solution for Your Anxiety Attacks!
If you are not fond of nature and nurturing plants, you may be shaking your head at the idea of gardening....
May 30, 2023 -
`
Health Benefits Of Eating Beets You Probably Didn’t Know
Beets have gained much importance as a healthy low-calorie food option in many diet charts. It has become one of the...
May 30, 2023 -
`
Best Books Ever Written About War That Every Man Should Read
Every military service member needs his daily dose of knowledge and skill enhancement, inspiration and motivation. And reading some books about...
May 30, 2023














You must be logged in to post a comment Login